

Clinical outcomes, such as ejection fraction, regional wall motion, risk of congestiveheart failure, and mortality, are al inferior with TIM12 flow compared withTIMI 3 f l ~ w.
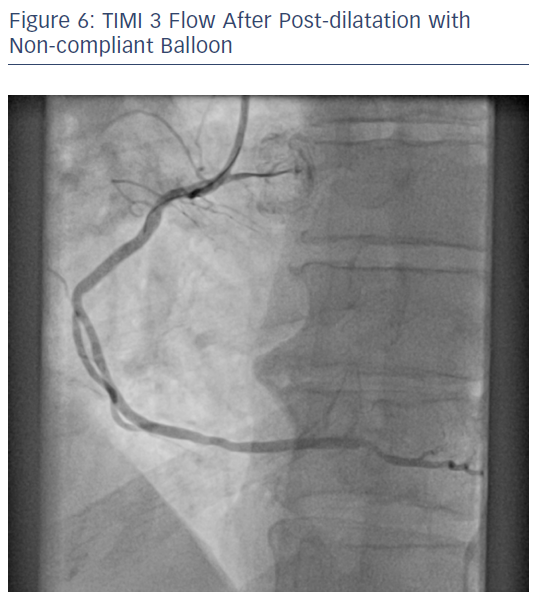
Subsequently, numerous trials have proven this categorization as faulty. TIMI 0/1 flow was deemed to be failure of âreperfusion,â while TIMI 2 and 3 flow grades were considered to be similar and denote successful repelfusion. The TIMI flow grades (Table I)â were established to provide a semiquantitative categorization of epicarclid blood flow, with the implicit assumption that this would reflect nzjocurdiul reflow. Despite the important differences in their meanings, these teims have unfortunately often been used interchangeablyto characterize the outcomes of MI therapy. âMyocardial perfusionâ is the ultimate goal and reflects the distribution of blood to the capillary and tissue level. The quality offlow has been quantified by TIMI flow grade since the early days of intravenous fibrinolyticreperfusion therapy. The ability to remove the occluding thrombus, by utilizing either fibrinolytic agents or mcchanical techniques, and thus open the IRA, is referred to as ârecanalizationâor establishing IRA âpatency.â âReflowâ is the visualizationof contrast dye flowing beyond the site of the previous obstruction to the distal vessel. Beyond EpicardidPatency Coronary atheroscleroticplaque rupture and thrombosis of a major epicardial vessel are the underlying cause of acute ST-segment elevation MI. In this review, we will attempt to clarify the confusion surroundingepicardialflow and ââmyocardialmalperfusion,âandprovide some insight into the next direction in acute MI therapeutics. In addition, we have promising treatments for prevention or alleviationof certain forms of microvascular obstruction. Techniques to evaluatebeyond TIMI epicardial flow are now available and validated.
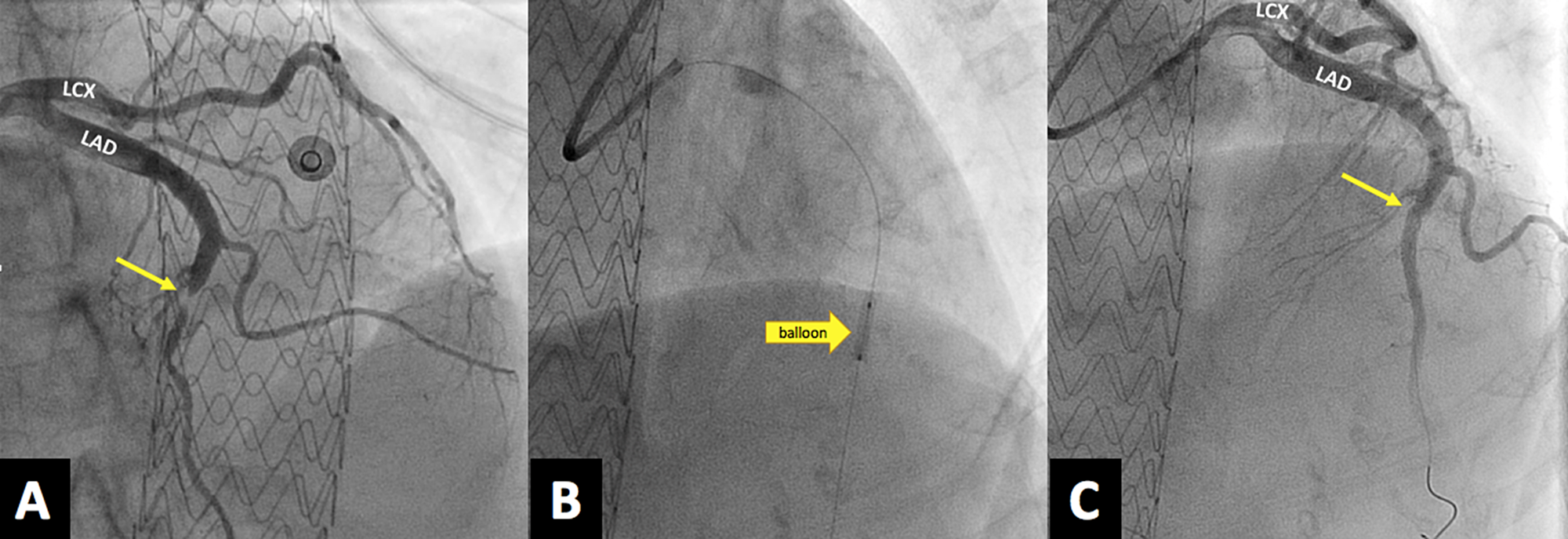
Key words: TIMI flow, perfusion, echocardiography,infarctrelated artery Introduction Combining low-dose fibrinolysis and platelet lysis appears to provide an additional increasein IRApatency,x-l but the largeI scale mortality reduction trials evaluating this strategy are just gettingunder way, Recently, considerable attention has shifted away from the epicardial arteries to the microvasculature.Contemporary evidence suggests that epicardial patency does not necessarily translate to actual perfusion at the myocardial level. This review attempts to clarify the confusion surrounding epicardial flow and âmyocardial malperfusionâ and to provide some insight into the next direction in acute myocardial infarctiontherapeutics. In addition, there are promising treatments for the prevention or alleviationof certain forms of microvascular obstruction. Techniques to evaluate beyond thrombolysis in myocardial infarction (TIMI) epicardial flow are now available and validated. Contemporaryevidence suggests that epicardial patency does not necessarily translate to actual perfusion at the myocardial level. Recently, considerableattention has shifted away from the epicardial arteries to the microvasculature. Combining low-dose fibrinolysis and platelet lysis appears to provide an additional increase in infarct-relatedartery (IRA) patency, but the largescale mortality reduction trials evaluatingthis strategy arejust getting under way. Jacobs Center for Thrombosis and Vascular Biology, The Cleveland Clinic Foundation, Cleveland, Ohio, USA Summary: Therapy for acute myocardial infarction has advanced dramatically since the early 1980s with the use of early intravenous fibrinolytic therapy. Reperfusion revisited: Beyond TIMI3 flow Reperfusion revisited: Beyond TIMI3 flowĬardiovascular Medicine, and *Department of Cardiology, Joseph J.


 0 kommentar(er)
0 kommentar(er)
